Some women are prescribed gabapentin for perimenopause or menopause symptoms, but it's important to realise the risks and alternative options
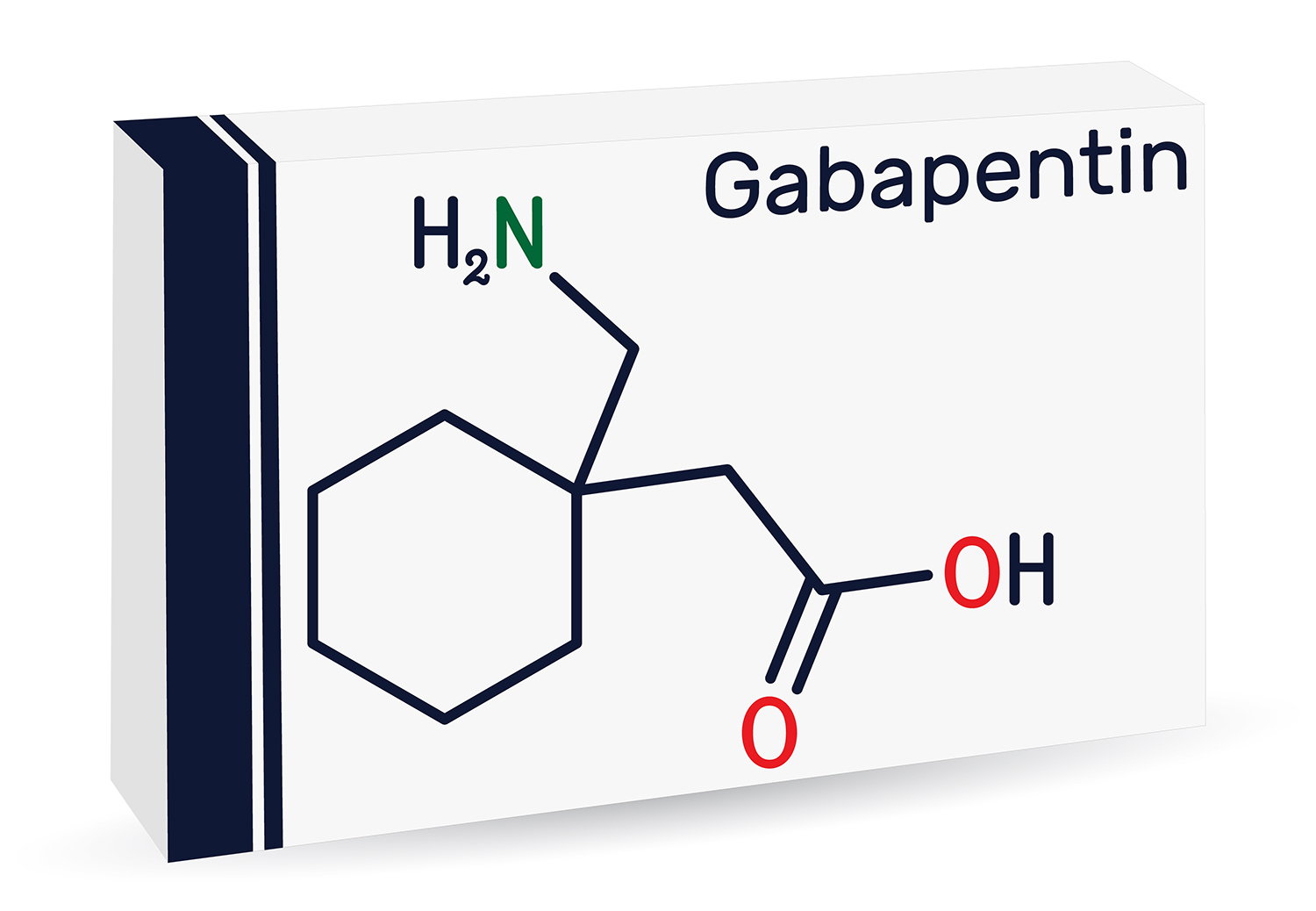
Gabapentin is a medication that's usually given to treat epilepsy or nerve pain. It is sometimes prescribed to reduce hot flushes. It is a prescription medicine and comes as tablets, capsules and liquid that you swallow. Brand names of gabapentin include Neurontin.
NICE menopause guidelines [nG23] don’t mention gabapentin and in the US, the FDA hasn’t approved official use of gabapentin for hot flushes. However, the International Menopause Society’s consensus statement says gabapentin can be considered if HRT is contraindicated or not desired for treatment of vasomotor symptoms.
How does gabapentin work?
Your body temperature is controlled by an area of your brain called the hypothalamus and when your hormone levels start to fluctuate and then fall, it can cause disruption in this area, which leads to hot flushes and night sweats. It’s not known exactly how gabapentin alleviates hot flushes but it’s thought it affects the thermoregulatory centres in the hypothalamus.
It takes at least a few weeks for gabapentin to work. A systematic review of gabapentin found it reduced hot flush frequency and severity compared to placebo. After four weeks, flush frequency decreased by an average of 1.62 episodes, and by 2.77 episodes after 12 weeks [1].
The review found that estrogen was more effective in reducing hot flush frequency than gabapentin. There was no significant difference in the reduction of hot flushes between gabapentin and antidepressants.
What are the side effects of gabapentin?
The most common side effects of gabapentin are drowsiness, light-headedness and dizziness.
Some people can become addicted to gabapentin, and it is associated with abuse – in one survey carried out at substance misuse clinics in Scotland, 22% of respondents reported they were abusing gabapentinoids [2].
Studies have found that gabapentin is associated with an increased risk of suicidal thoughts and behaviour [3,4]. A recent study of the 20 medications most commonly associated with suicidal ideation and self injurious behaviour included anti-epileptics (gabapentin and pregabalin) - it found that these had the most reported adverse events in those aged 51-55 [5].
If you decide to come off gabapentin, you’ll need to reduce your dose gradually to avoid withdrawal symptoms such anxiety, nausea and difficulty sleeping.
Talk to your healthcare clinician about any side effects you are experiencing.
Who can take gabapentin?
Gabapentin may not be suitable if you’ve previously been addicted to a medicine.
You may not be able to take it with strong painkillers, some antidepressants and antipsychotics and malaria prevention drug mefloquine. If you take antacid, take it at least two hours before or after gabapentin.
Gabapentin may not be suitable if you are on a controlled sodium or potassium diet or if your kidneys don’t work well.
What’s the bottom line?
The most effective evidence-based treatment for perimenopausal and menopausal symptoms, including vasomotor symptoms, is HRT, because it targets the underlying cause. Also, HRT is bone, heart and neuro-protective, and reduces all-cause mortality by 30% [6].
It’s worth remembering that perimenopause can last up to 10 years and that, unlike HRT, gabapentin will not treat the myriad of potential symptoms you may experience. Unlike HRT, it will not help improve your future health or lower your risk of future diseases.